
Cureus Ocular Complications in Patients on Highly Active
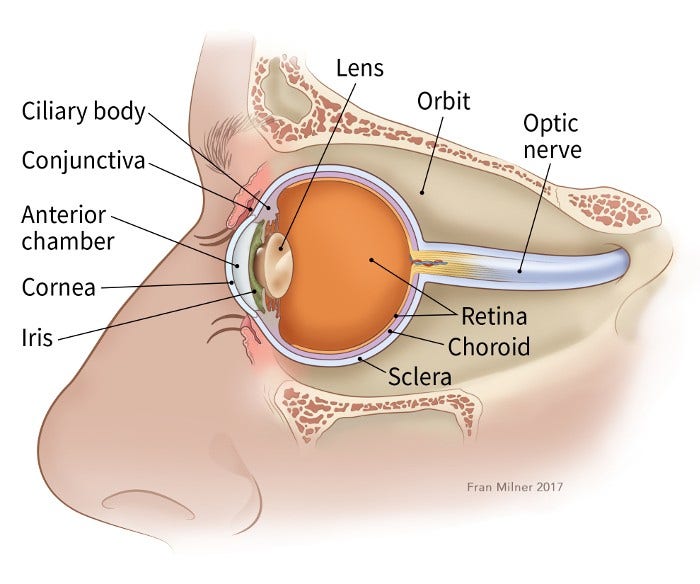
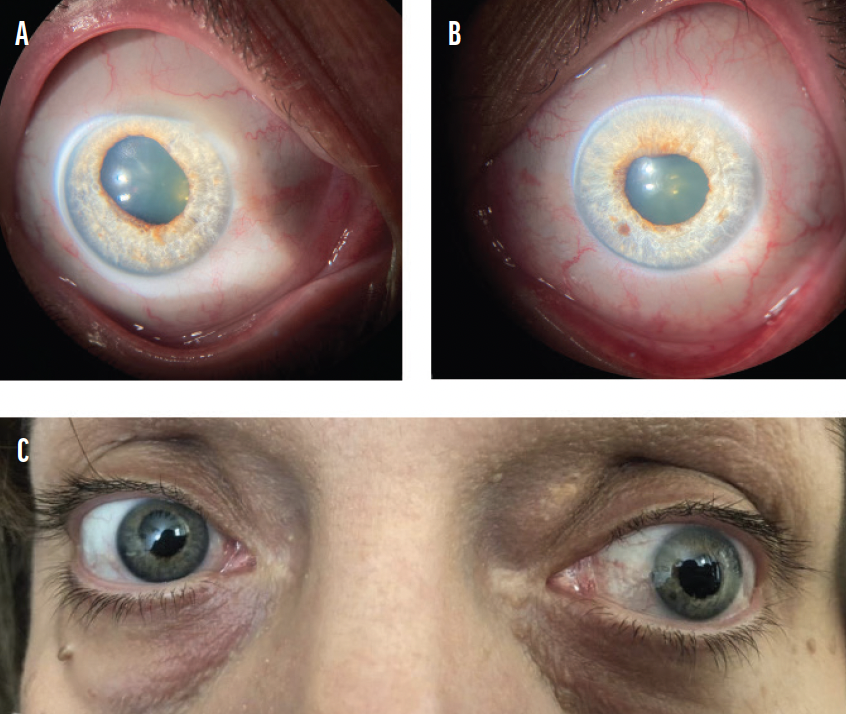
Our article aims to report the ocular adverse effects of highly active antiretroviral therapy (HAART). In case 1, a 26-year-old male patient presented with a diminution of vision. In the absence of active cytomegalovirus (CMV) retinitis and a surge in CD4 count of more than 100 cells/µL over four months, he was diagnosed as a case of immune recovery uveitis (IRU). He responded well to topical steroids and cycloplegics. In case 2, while dry eye is a common adverse effect of HAART, our 53-year-old female patient progressed to a visually distressing stage of keratoconjunctivitis sicca. She responded to lubricants and continues to be on the same. In case 3, a 14-year-old female patient’s vision succumbed to Stevens-Johnson syndrome due to nevirapine in the absence of timely intervention. Though uncommon, debilitating ocular adverse effects may be seen with HAART. Further studies and reporting are required for an increased awareness among physicians and patients.
If Your Child Has Retinoblastoma

Frontiers A new era for optic pathway glioma: A developmental brain tumor with life-long health consequences

Why Is PRK Safer Than LASIK?

How Does Rheumatoid Arthritis Affect the Eyes?

What Causes Red Eyes & How to Get Rid of Stoned Eyes Fast

Eye drop recall stirs concern about over-the-counter drug safety

LipiFlow® Thermal Pulsation System: A New Dry Eye Treatment for MGD - Johnson & Johnson

PRK vs. LASIK: Which Procedure Is Best for You?
The Ocular Manifestations of COVID-19 - Glaucoma Today

The Curious Case of Natalia Grace: Where is she now? - Dexerto

A Curious Mind Expanded Edition: The Secret to a Bigger Life: Grazer, Brian, Fishman, Charles: 9781668025505: : Books
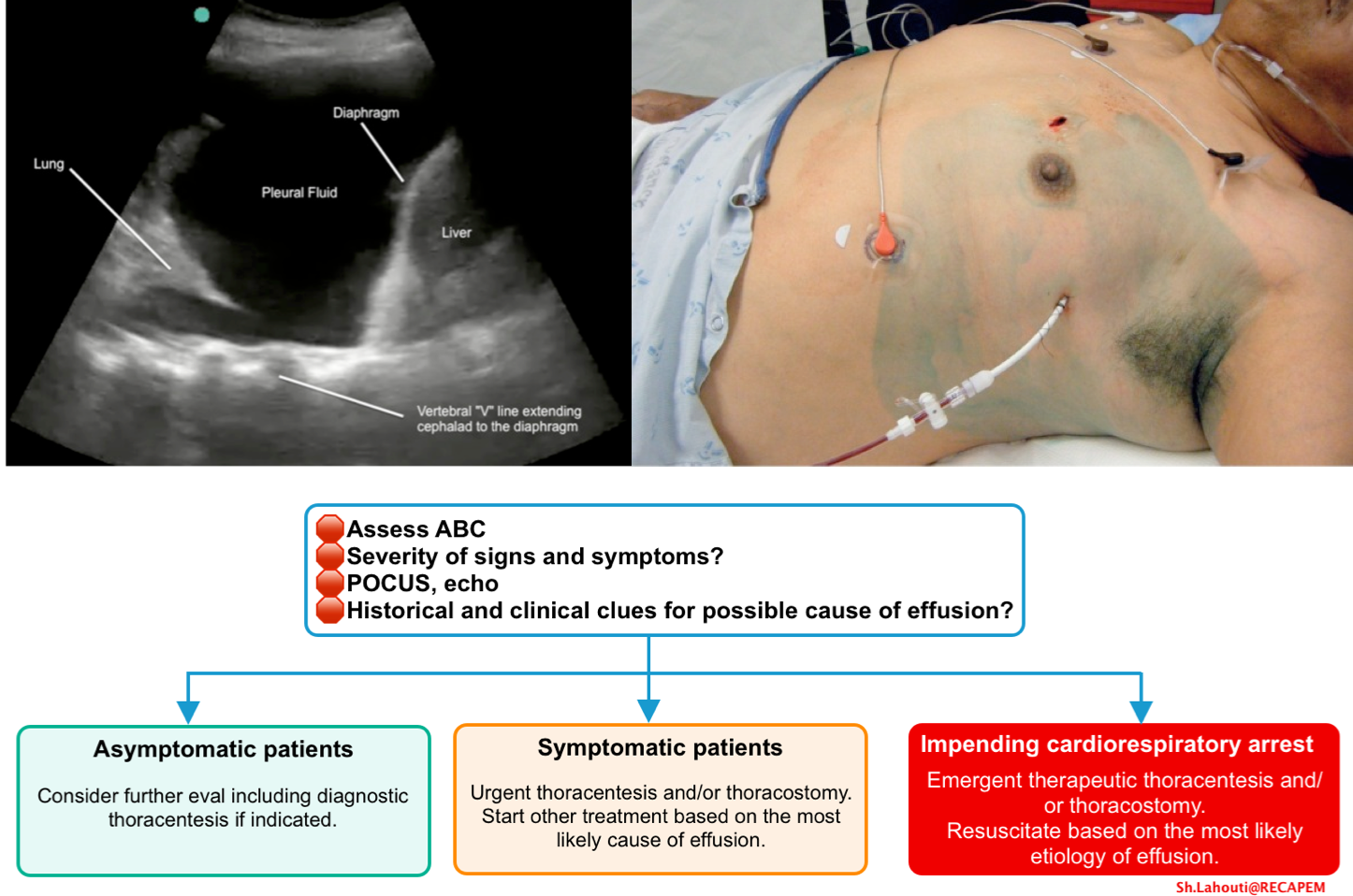
Pleural Effusion In Critically ill Patients
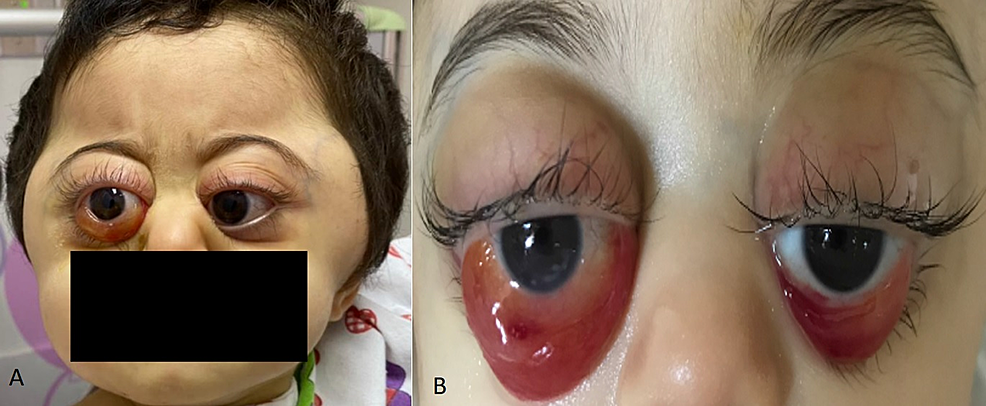
Cureus, Rapidly Progressive Ocular Proptosis as the First Sign of Neuroblastoma in a 16-Month-Old Child: Case Report and Review of Literature

Updated Diagnostic Criteria for Paraneoplastic Neurologic Syndromes








